Webinar highlights: Digital Applications in Mental Health
Ahead of the World Mental Health Day celebrated every 10 October, seven huge EU projects brought together experts for the second episode of Mental Health Dialogues. How do these projects address common issues in digital applications in mental health support such as designing with data privacy and human-in-the-loop in mind, as well as sustaining motivation to use such digital interventions?
Together with mental health and digital innovation experts of seven big Horizon Europe projects, the Mental Health Dialogues series held on 4 October 2024 tackled some of the most important questions commonly encountered by both the scientific teams and users.
The following presents the highlights of the panel discussion:
Recent studies reveal growing user scepticism towards digital applications, particularly regarding data privacy. How does your project address data privacy and security for users interacting with your digital tools?
-
Emphasise safety and security through clear communication, ensuring that users are well-informed about how their data is protected. This includes using encryption, secure login methods (e.g., PIN codes), and delivering private information through secure channels like messaging modules.
-
Build trust by providing transparent and accessible privacy measures. While offering users control over their data is important, the system should balance responsibility to avoid overwhelming users with complex data-sharing options. Privacy by design should be a priority from the early stages of development.
-
Incorporate feedback from users during the design phase to ensure that privacy measures address their specific concerns. Limit the collection of personal data by using predefined responses and minimal data collection. Security features such as password protection and limited information in notifications help maintain user privacy.
-
Implement creative methods, such as using random data (e.g., GPS) to protect privacy. Provide educational materials to help users understand privacy safeguards. These can include videos or guides to increase awareness and confidence in the system's security measures.
-
Adhere to data protection regulations, such as GDPR, and integrate ethical standards from the outset. Secure personal data through robust authentication, encryption, and dedicated servers. Dynamic authorisation and anonymisation techniques, such as using avatars, can further protect user identity and encourage participation.
-
Ensure privacy is a foundational element of system design. Develop ethical frameworks through stakeholder input, focusing on collective rather than individual personalisation. Secure data storage on local, restricted-access machines can help minimise the risks of exposing sensitive information.
-
Empower users by giving them control over their data and ensuring they understand that participation is voluntary. Stakeholder meetings can help develop effective communication strategies about data privacy, fostering a sense of security and trust.
Ensuring sustained user engagement is a significant challenge in digital mental health interventions. How does your project design applications that not only motivate initial use but also support long-term adherence, while aligning with both technical requirements and medical protocols?
-
Involve stakeholders throughout the development process to ensure the intervention is relevant and tailored to users' needs. Offer a range of choices and customisation options to allow users to focus on what matters most to them, fostering a sense of ownership and engagement.
-
Address motivation and self-efficacy to prevent drop-out by providing regular, individualised feedback that reinforces progress. Consider user preferences and contexts when designing interventions to maintain relevance and long-term participation.
-
Incorporate interactive features like notifications, gamification, badges, and rewards to make the experience more engaging. Use these elements to spark curiosity and provide users with fun and light-hearted content that maintains their interest over time.
-
Acknowledge that user engagement strategies may vary depending on individual preferences. Experiment with multiple approaches and adjust based on user feedback and data. Ensure the data collected remains meaningful, even when using techniques like gamification to boost adherence.
-
Create applications that are easy to use and navigate, enhancing the overall user experience. A seamless, intuitive interface helps sustain engagement, making it easier for users to recognise the benefits of participation.
-
Use algorithms and contextual data collection to tailor the user experience further. Analyse user preferences and feedback to adjust exercises and support systems dynamically, keeping the intervention aligned with their evolving needs.
-
Consider implementing initial "engagement calls" or other forms of onboarding that allow users to ask questions and set expectations. This can help reduce uncertainty and build a stronger connection to the intervention from the start.
-
Ensure that the focus on engagement and rewards does not compromise the integrity of the data collected. While incentivising participation is important, maintain a balance to ensure high-quality and useful data for analysis.
While digital tools offer valuable possibilities for mental health support, the role of human healthcare professionals remains crucial. How does your project integrate human expertise and oversight alongside digital interventions and ensure that human practitioners are involved when necessary?
-
Digital interventions should be designed to complement, not replace, human healthcare professionals. They can assist by enhancing assessment, follow-up processes, and supporting clinical decision-making, but the ultimate responsibility for treatment should remain with the healthcare professionals.
-
Develop digital tools through a co-creation process involving healthcare professionals and other stakeholders, such as teachers or family members. This collaborative approach ensures that interventions align with real-world needs and are grounded in professional expertise.
-
Adopt task-sharing models where non-specialists, such as trained educators or community health workers, collaborate with specialists. Non-specialists can deliver parts of the intervention under the supervision of mental health professionals, making the system more scalable while maintaining quality oversight.
-
Mental health professionals should take on supervisory roles, overseeing and training non-specialists who deliver interventions. This ensures a consistent standard of care and enables specialists to intervene when necessary.
-
Utilise patient-reported outcome measures, ecological momentary assessments, and other real-time data collection tools to provide ongoing feedback to clinicians. This enables professionals to make informed decisions and adjust interventions based on real-time insights.
-
Recognise that both guided and unguided interventions have value. While guided interventions may offer more tailored support, unguided self-help approaches can provide scalable solutions, especially for users with lower symptom levels. Consider a mix of both to cater to different needs.
-
Design digital systems with built-in empathy and personalised support. Encourage users to provide subjective observations through reflective exercises, which can enrich the data and allow healthcare professionals to make more empathetic and tailored recommendations.
-
Even in primarily digital interventions, human involvement should be available for crisis situations. While some digital tools may promote autonomy and self-help, human oversight can significantly enhance effectiveness, particularly during moments of heightened need or crisis.
-
For large populations, fully digital interventions without human involvement may be necessary to ensure scalability. However, these should still emphasise promoting health and autonomy, teaching users to manage mental health issues independently where appropriate.
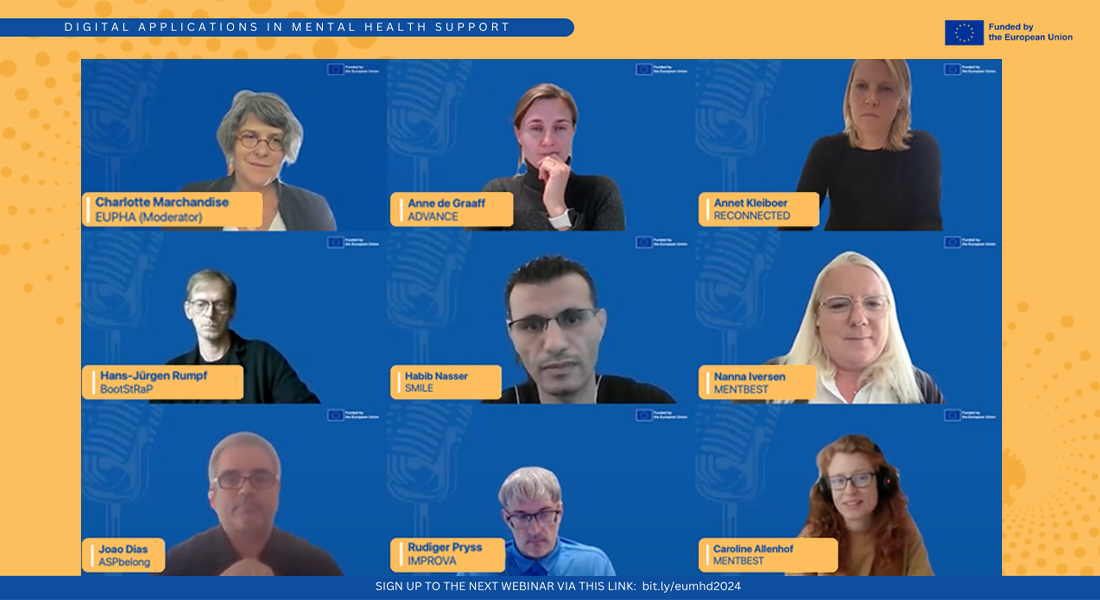
Attended by over 100 participants consisting of researchers, practitioners, people with lived experiences, association representatives, and policy-makers, the interactive session has gathered valuable inputs both from the panelists and the attendees. This webinar is also held in close collaboration with the European Health and Digital Executive Agency (HaDEA) - the funding agency of the seven EU projects - as a way to influence policy and future programmes.
The event was opened by Stéphane Hogan, Head of Health Research Unit of HaDEA and was moderated by Charlotte Marchandise, Executive Director, European Public Health Association (EUPHA). The expert panelists include Anne De Graaff (ADVANCE); Habib Nasser (SMILE); Caroline Allenhof (Mentbest); Annet Kleiboer (Reconnected); João Dias (ASP-Belong); Hans Jürgen Rumpf (BootStRaP); and Rüdiger Pryss (Improva).
"Mental Health Dialogues" is an initiative of 7 big EU Horizon Europe projects under boosting mental health in Europe in times of change (HORIZON-HLTH-2022-STAYHLTH-01-01-two-stage), namely ADVANCE, ASP-belong, Boostrap, Improva, Mentbest, Reconnected, and SMILE. This is the first of a 4-year joint-webinar project with the aim to provide synergy among like-minded mental health research serving Europe and beyond.
Contact:
Joyce Anne Quinto
Project and Communications Manager
joyce.quinto@sund.ku.dk
